HIP ARTHRITIS
HIP REPLACEMENT
WHAT IS ARTHRITIS?
The commonest cause of pain in old age is degeneration, where joints have simply worn over years. This is known asosteoarthritis. Hip is the second most frequently affected joint. 11% of England’s population over age of 45 have treatment for hip condition.
Other conditions such as inflammatory arthritis (either rheumatoid or psoriasis), childhood hip conditions and severe injury to hip joint or pelvis can also lead to secondary hip arthritis.
HOW DOES IT PRESENT?
You will notice pain around hip and stiffness. You may feel pain in the groin area and in the front of thigh going down to the knee (like hand going in the pocket). Sometimes you may feel pain around the side of hip or in the buttock.
You may typically notice pain on weight bearing. Walking ability slowly starts going down. 18 hole golf may become 9 and shopping can become a chore!You may notice pain at night or on turning in bed.
Finally you may not be able to reach your toes, shoes or socks. You may find it difficult to get in and out of bath, car and low chairs.
HOW IS IT DIAGNOSED?
Your history and examination is usually sufficient to make a diagnosis. I will check your gait, hip movements and rest of the leg. Occasionally pain from lower back can mimic hip pain. Therefore, if in doubt, I will check back as well.
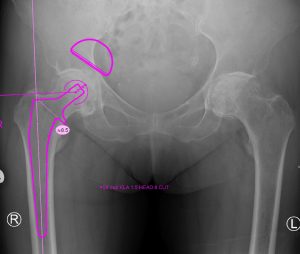
X-ray of both hips will confirm if you have arthritis. In most cases further investigation such as a scan is not needed.
WHAT DOES THE OPERATION INVOLVE?
I perform operation mostly under spinal (needle in the back to freeze legs) or rarely under general anesthesia. Please discuss your options with the anaesthetist. You can go to sleep or have general anaesthesia on top of spinal (so that you do not hear saw and hammer!). Or you can choose to listen to your music while operation is under way.
Once under anaethesia, you will have a catheter in bladder (so that
you are comfortable at night). We will position you so that you are lying on side. We will remove hair on side of hip if necessary and clean the leg with antiseptic solution.
I will make a cut on the side of the hip. I will expose the worn joint and remove the damaged part of thigh bone (femoral head). I will prepare the socket (acetabulum) with cheese grater type reamers. I will implant the artificial socket with bone cement.
I will then prepare, wash and dry thigh bone (femur). I will implant the artificial femur stem and head. After making final checks, I will close the wound and apply padded dressing.
WHAT IS THE TREATMENT?
Hip arthritis treatment initially includes:
- Pain killers
- Anti-inflammatory medication (Local Gel or Tablets)
- Weight loss
- Walking aid
- Physiotherapy (range of motion exercises, aerobic exercises and strengthening exercise)
Injection of steroid in the hip joint can be considered in some cases.
If pain cannot be controlled by these methods and if it affects activities of daily living, quality of life; then hip replacement is a good option.
WHAT ARE THE RISKS AND COMPLICATIONS?
Hip replacement has become a standard orthopaedic operation. It is ranked the best operation to improve quality of life amongst all operations. It is excellent at reliving arthritic pain.
It has some risks and complications. However most patients are delighted with the results.
Possible complications specific to hip replacement include
- limb length discrepancy (one leg longer than other),
dislocation, - failure,
- damage to nerve or blood vessels.Other complications are:
- small risk of clot in leg (DVT) or clot breaking loose (PE),
- pain,
- swelling,
- bleeding,
- revision surgery in case of wear or failure.
WHICH HIP DO YOU USE?
I use Corail hip or Exeter hip. Both have good reproducible long-term results. I have trained in the Exeter hip Unit. It can truly be said that this prosthesis has stood the test of time and its long-term results are outstanding. Similarly Corail hip has been in use for over 25 years with excellent results.
Both are not a metal on metal hip.
WHAT IS THE RECOVERY?
Soon after the operation (after ‘legs come back to life’), you can start exercises to keep ankles and calf active. You will have stockings on both legs. Physio will teach you how to use a walking frame. As soon as you master walking with frame, physio will move you to crutches. Once you can walk down the corridor and master stairs, you are ready to go home!
You will need someone (adult) at home with you for about six weeks. You will also need some special modifications to bed, chair and a raised toilet seat. (This will be arranged prior to your discharge).
You will have a wound review and removal of clips at two weeks and I will see you at six.
You can walk as far as you want once comfortable. It may be preferable to use a stick or hiking pole for long distances. Use shower for first six weeks instead of bath. Swimming, dancing and light gym work such as bike or treadmill can be started after six weeks.
You may return to sedentary (less active) work by six to eight weeks. People with heavier jobs can return back in about three months with some alteration to duties. Driving is not permitted for first six weeks. Avoid all non-essential car journeys for the same time.
Air travel is best avoided for three months.